Overworked Sydney intensive care nurses are increasing sedative doses for some patients in order to manage their workload, claiming pressure from the Delta outbreak makes it impossible to monitor all of their charges.
Two ICU nurses from Sydney’s Royal Prince Alfred and St Vincent’s hospitals have independently raised concerns that when working in non-Covid ICUs in recent weeks, the pressure that surging Covid cases had placed across the health system has left them understaffed to the point that increasing sedative dosage is the safest way they can manage their patient load.
Guardian Australia does not suggest the nurses have administered sedatives their patients were not already prescribed by a doctor.
Rather, the ICU nurses, who oversee the infusion of sedatives and administer varying levels within a certain dose range prescribed by a doctor – known as titration – report that when staff are stretched, decisions have been made to increase sedation to the maximum allowed dose “to knock the patient out” so nurses can ensure the patient will remain safe when they need to divert their attention elsewhere.
Royal Prince Alfred hospital acknowledged it was currently a “challenging time” for the hospital, with surge workforce plans in place, while St Vincent’s said its ICU is “well resourced”.
Neither hospital addressed specific questions about sedation asked by Guardian Australia. However the New South Wales Nurses and Midwives’ Association has maintained that the NSW health system has not been staffing ICUs to meet professional standards, and say the understaffing was a problem before the pandemic but that it has become significantly worse during the Delta outbreak.
In examples given by the nurses, who have not been named to avoid them being identified, they say patients already receiving a low level of sedation who are in unclear states of consciousness, and may be at risk of fiddling with their breathing machine or other apparatus, might have their sedation increased so they don’t dislodge tubes that could cause significant damage.
They report this is occurring when they have two or three patients they need to monitor including one on ventilation – above the desired ratio of 1:1.
They claim the Delta outbreak and associated staff pressures have made this decision more common.
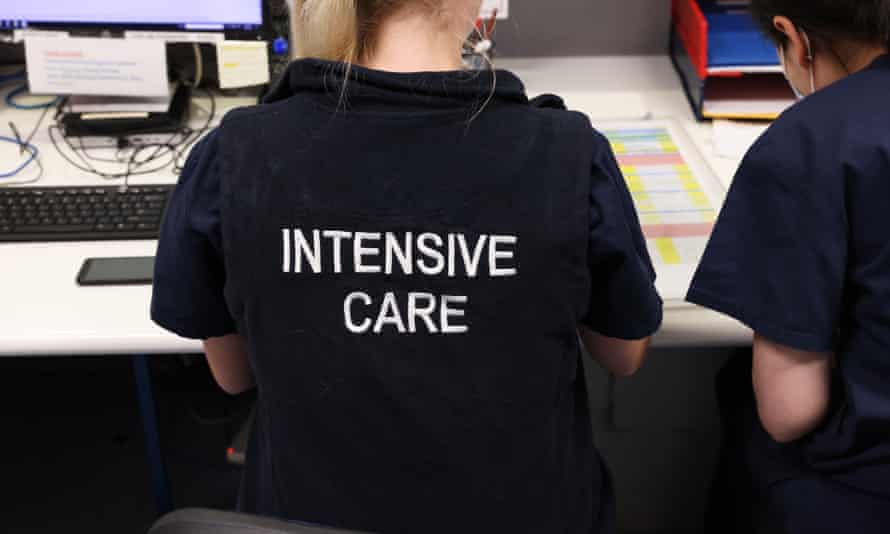
The nurses claim that in a well-staffed ICU, a nurse would be designated to constantly monitor a ventilated patient, and the patient would otherwise not have their sedative dose maxed out.
The nurses, who have asked to remain anonymous, contacted Guardian Australia concerned with how health authorities were portraying the state and preparedness of NSW’s ICU capacity at daily Covid updates.
Their comments follow broader concern from healthcare workers that while the NSW government may be correct in its claims it can expand ICU capacity to 2,000 ventilated beds across the state, there is insufficient staffing and training levels to care for each one of those beds.
On Sunday, there were 813 Covid patients in hospitals across NSW, 35 more than Saturday and 256 more than the previous Sunday.
There are now 126 people in intensive care, with 54 on ventilators. Of those in intensive care, 113 had not received any vaccine doses, while 12 had received one dose and one patient had been double vaccinated.
Sign up to receive an email with the top stories from Guardian Australia every morning
Reports of NSW’s current ICU capacity are varied. While NSW Health has said the base of 500 ICU beds was currently being expanded, it was reported that as of Wednesday, there were 845 beds across public and private hospitals, with 667 of those occupied. About 17% were Covid patients, however the number of Covid patients in ICU since then has increased by 10.
National cabinet has reportedly received a briefing that warns NSW does not have sufficient skilled staff to operate every bed in its expanded ICU capacity, according to the Saturday Paper.
Covid patients spend more time in ICU than other patients.
While attention has been focused on ICU capacity for a growing number of Covid patients, nurses report care in non-Covid ICU and other sectors is being affected as staff are seconded to Covid specific units, forced to isolate after exposure, or leave to work at vaccination clinics.
One of the ICU nurses who spoke to Guardian Australia, described the ICU environment at one of the hospitals as a “hellhole” in recent days. The nurse has worked in ICU for several years, and claims it is currently “the busiest I’ve ever seen it”.
Regarding titration of sedatives, the nurse said that because of staffing pressures, “If someone is busy or something happens elsewhere, you turn up the sedation dose to knock the patient out so you can move elsewhere and know there won’t be a problem if you’re not keeping eyes on the patient.
“It’s a bad thing because you want the patients to do more breathing on their own, but I know that if I up the sedation they will be safe from dislodging things like ripping out tubes which could be significantly worse for their health than me sedating them for a few hours.
“If we deem it necessary, then we up it, just in the same way we can lower it if we sense a chance for them to come off ventilation. There’s no questions asked at the moment.”
The nurse stressed that increasing sedative dosage during current staffing pressures can be the safest outcome for patients. The nurse offered the example of a patient who had recently dislodged a feeding tube while unsupervised and it had moved into an airway pipe and moved into his lung.
“If a nurse had been watching overnight that wouldn’t happen, but when nurses have to monitor more than one patient in ICU, especially if one is on ventilators, you just can’t see all the patients at once, there are walls and partitions.
“If there’s not enough staff it’s just significantly more dangerous.”
The nurse was also sceptical of how new ICU beds would be staffed, noting the skills required to operate equipment in ICUs took him months of training.
“There just aren’t the bodies and there isn’t the skill in here to cope now. And a lot of colleagues are quitting recently, when they can just go and get a job in a vaccine clinic, because you’re paid more doing that and ICU is not a fun place right now.”
The nurse reports receiving multiple texts each day from his hospital pleading for staff to take on extra ICU shifts. Texts this week, seen by Guardian Australia, noted some shifts were 16 ICU nurses short.
“When you see those messages and you’re 16 people short and you’re coming in that night, you know you’re coming in for an awful shift, you think, why would I want to come in for a shift in that hellhole?
“And when you do go in for extra shifts, you’re knackered and you aren’t as good for your regular shifts.”
The nurse has worked shifts recently with retired and ex-ICU nurses who have been recalled into the system. In addition to more skilled ICU staff,they want to see more unskilled labour brought in to help with things such as stocking storage units and taking out filled bins – something the nurse has noticed have fallen behind recently.
Another ICU nurse who spoke to Guardian Australia, was also concerned that nurses were being forced to “lean” on higher sedation doses within prescribed ranges because of staffing shortages.
The nurse described similar situations concerning patients fiddling with tubes while ventilated, and being too stretched to monitor them.
“We shouldn’t be leaning on these practices in place of adequate staffing,” they said.
“Already I’ve seen a heavier reliance on chemical restraints to manage risky behaviour in the ICU patients … If we were staffed better, I don’t think we would have had to do that,” the nurse said, adding that they felt worried about how their ICU would cope as the Covid outbreak worsened and staff were further stretched.
Michael Whaites, manager of the public health organising team within the nurses union (the NSWNMA), said nursing in NSW had been understaffed since before the pandemic, including failing to meet ICU standards for staffing.
He said he had heard of 1:1 ratios for ventilated ICU patients not being met.
When asked about changes in sedative reliance among nurses during Delta, Whaites said: “We haven’t had reports of that made to the union. We know nurses have been raising issues about staffing since before Delta and Delta is making it so much worse. What nurses have to do is make decisions about their patients’ safety they’re directly responsible for, that’s their professional obligation,” Whaites said.
Hospitals’ response
A spokesperson for Sydney Local Health District, which oversees RPA hospital, told Guardian Australia: “Staff are working extremely hard to care for Covid and non-Covid patients admitted to RPA’s intensive care unit (ICU). Multidisciplinary teams – including doctors, nurses and allied health staff – are working together daily to ensure patients continue to receive high quality care in a safe environment.
“Under the existing model of care in RPA’s ICU, patients who require ventilation have a dedicated nurse overseeing their care. During this challenging time – and as part of the response to the pandemic – there are workforce surge plans in place across the district,” the spokesperson said.
David Faktor, spokesperson for St Vincent’s hospital, said its “ICU is currently well resourced to contend with the anticipated patient load requiring critical care”.
“In recent times the hospital has been running courses to upskill some additional nurses to work in ICU to ensure the unit has the ability to scale up its capacity if need be – while not compromising the skill mix required to support the unit’s highly complex and acute workload.
“The hospital has had no formal concerns raised by any staff through our various channels, nor have we had any reported adverse incidents. St Vincent’s has a workplace culture of strongly encouraging staff to come forward with any clinical concerns – and has a number of mechanisms in place for staff to do so,” Faktor said.
Do you know more about how Sydney hospitals are responding to pressure from the Covid outbreak? Contact elias.visontay@theguardian.com You can remain anonymous.